Covid-19 Irish Medical Professionals Attack Lockdowns – Full Text – Share…
This newly-released document by Irish Medical Professionals, released on November 15th, outlines what the Irish Government and NPHET have known since March – that lockdowns kill far more people than they save. We have distilled the document down and made it more readable, with jump-links below to individual sections for your convenience.
This move by Irish doctors echoes the September address by 60 US Doctors at the US supreme court, which we linked for you in our Covid-19 information section here.
Share it far & wide, let’s bring back reality to the masses.
Below is the full text of Nov 15th’s Whitepaper release by actual Irish Medical Professionals. Remember, no one in NPHET is an actual medical professional, yet the compromised Irish Government has outsourced complete control of the country to them. The political opposition in Ireland has gone along with everything and asked no questions – Sinn Fein, and PBP are both complicit.
These Irish Doctors put it far more diplomatically that we do. We say NPHET and many members of the Irish Government should be tried for Crimes against Humanity.
Send this to anyone you think may be on the cusp realising we have been lied to on a monumental scale. All numbered references in the paper can be found on the original document linked at the bottom (number 8)
Jump Links to section ↓
- Introduction to an alternative Covid Strategy for Ireland
- Lockdown Interventions – are there convincing real-world benefits for morbidity / mortality?
- Lockdown Interventions – what is the evidence for costs exceeding benefits?
- General Impact on hospital system and elective care
- Lockdown Impacts on Cardio, Cancer, & Mental Health
- Is PCR testing an appropriate tool to inform policy?
- Proposing an evidence-based path forward
- References and Doctor Signatory list (forward to your doctor)
COVID-19 Alternative Strategy – A Case for Health and Socioeconomic Wellbeing
Introduction:
Ireland is currently living through a once in a generation crisis. A new virus, SARS-CoV-2, which causes the disease COVID-19, swept the globe in the late Winter and Spring of 2020. We put in place an intuitive mitigation measure: the initial ‘Lockdown’, in an effort to ‘Flatten the Curve’. This was a natural and appropriate response which bought time by slowing the progress of COVID-19 through our community. This protected the vulnerable, our healthcare workers and our health system. We believe that the initial epidemic phase passed in early Summer of 2020 and that the virus is now establishing itself as an endemic virus like many before it.
We must now develop strategies that acknowledge:
- the ongoing morbidity and mortality among our population caused by COVID-19
- the undeniable impacts on our ability to provide routine and acute health services.
- the now greatly reduced risk of overload in our health system.
- the context for COVID-19 when compared to all other healthcare demands.
- all of the other crucial aspects of a functioning society negatively impacted by current strategy.
A failure to update the strategy for managing the virus and its impacts is at risk of becoming the main driver of harm in our society. The scientific and medical understanding of COVID-19 has evolved enormously since early 2020: it is now possible to be very precise in predicting which populations are most vulnerable to infection with SARS-CoV-2; it is now clear how this virus differs in behaviour and effect to other common pathogens such as Influenza; there is a much greater understanding of infection fatality rates (0.23% across all groups and jurisdictions)1since early modelling from the Imperial College group; seasonality; viral dynamics; the futility of unfocussed track and trace; problems with mass PCR testing and much more.
In this White Paper, we aim to promote an improved understanding of the current strategy, focussing on cost-benefit dynamics. With scientific analysis of the topics listed below, we propose a set of a viable and potentially more advantageous alternatives, in an effort to assist policy makers with the difficult decisions ahead.
We initially address the latest evidence for lockdown efficacy and examine the enormous and, in our view, disproportionate cost of cyclical lockdown in terms of health, economic, and societal damage. We also address the weakness of the test and trace system in its current format, and the use of theoretical modelling in setting policy.
Firstly, let us briefly take stock of the current situation, with the benefit of 8 months of experience:
- Mortality impacts from COVID-19 are now known to be within the envelope of previous recent significant respiratory seasons (e.g. 2000, 2015, 2018) 2.
- Current pressure on hospital and ICU beds is comparable to previous winters.
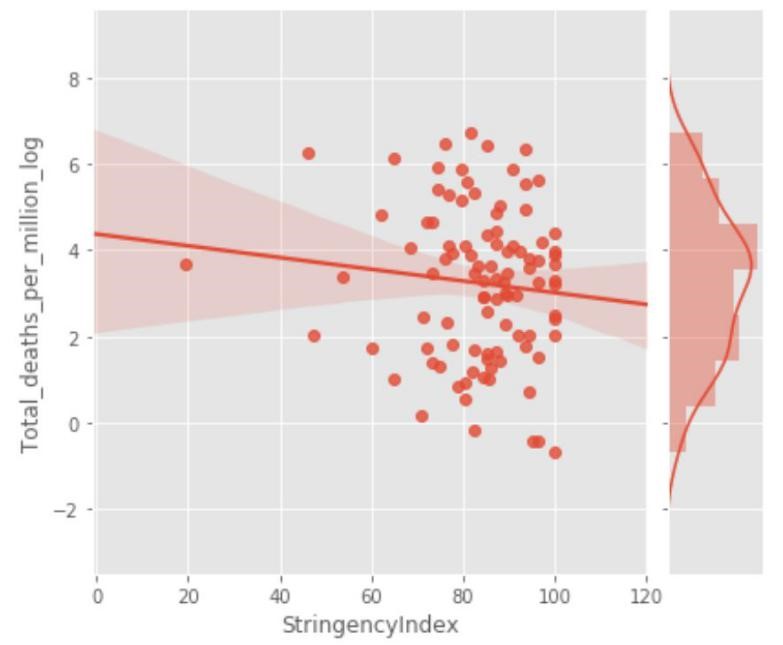
- Lockdown has not previously been employed as a strategy in pandemic management, in fact, it was ruled out in 2019 WHO and Irish pandemic guidelines,3and as expected, it has proven a poor mitigator of morbidity and mortality (fig. 1).
- “Test and trace” becomes overwhelmed and loses effectiveness after a virus has substantially entered a population (up until 2019 it was not recommended by the WHO for this very reason) 3. Tactical testing may still have a role e.g. for workers and residents in key environments such as nursing homes etc, ideally using dependable antigen testing rather than PCR. We believe that the virus is on its way to being endemic, and recommend that testing be reorganised and focussed in conjunction with clinical case evaluation, as per pre-existing WHO and Irish pandemic guidelines.
Lockdown Interventions – are there convincing real-world benefits for morbidity / mortality?
The original purpose of lockdown was to “flatten the curve”, protect hospital capacity for the provision of ongoing non COVID-19 care and reduce morbidity and mortality from COVID-19. Confidence in this strategy was based on reasonable assumptions, modelling and forecasts derived from the available data in the spring of 2020. We now have the benefit of experience and multiple published analyses reflecting real-world data and outcomes. A recent paper in The Lancetshowed no correlation between lockdown measures and mortality outcomes: “Rapid border closures, full lockdowns, and wide-spread testing were not associated with COVID-19 mortality per million people”.4Notably, a large number of published preprint analyses converge on lockdowns having a minimal beneficial effect on mortality outcomes.5678910
There is a dearth of published evidence indicating that lockdowns reduce overall mortality; a significant concern in itself, given the enormous negative impacts of lockdown. Sweden is particularly notable as a “control” country which largely followed the 2019 WHO Pandemic Guidelines, rather than pursuing the very new lockdown approach.
With this strategy, they experienced a similar mortality impact to other European countries, when various key factors are accounted for. Below we see that Sweden had a relatively tiny impact compared to the Spanish Flu of 1918, and one which hardly stands out from more recent years (fig. 2). On current data, Sweden will essentially have a “normal” excess mortality in 2020 – with no real signal emerging versus prior years. Regardless of lockdown intervention, Ireland also exhibits no excess mortality versus prior years, even when zoning in on the first five months of the year (fig. 3).


The most recent Level 5 Lockdown in Ireland was implemented on the basis of “modelling” projections from “PCR-positive case trends”. It was also driven by an apparently excessive increase in Covid-19 hospitalizations and ICU occupancy. Reviewing the real-world data, it is clear that when adjusting for lag, the lockdown came well after the rate of infection and hospitalization had already been falling substantially11 (fig. 4).

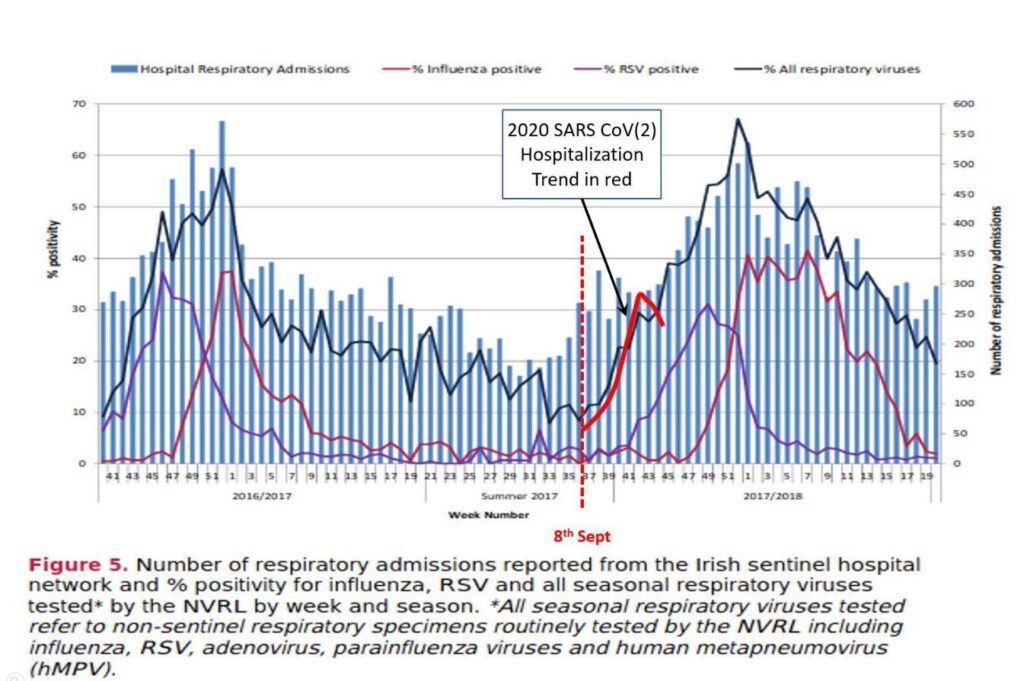
In terms of the concern around hospitalizations and ICU trends where a positive PCR was recorded, there was no substantial difference when comparing to prior years. In figure 5, the superimposed red line approximates the trend for PCR-positive hospitalizations in 2020 before the level 5 lockdown was imposed. In essence, the numbers are not out of step with the trends seen coming into winter 2018.
Lockdown Interventions – what is the evidence for costs exceeding benefits?
It is critical that we now apply our understanding of these analyses and ask the question: Do the costs of lockdown outweigh (possibly greatly) – the benefits of lockdown? A recent paper published in the British Medical Journal concluded that lockdown interventions could increase COVID-19 mortality rates over the long term.12Another analysis in preprint proposes the same unintended consequences.13
It is crucial that we consider these latest analyses, and face the possibility that lockdown interventions could result in more COVID-19 deaths than if we simply followed the WHO 2019 pandemic guidelines, as Sweden did.
Lockdown significantly undermines many elements of public health. As a strategy it is detrimental to breast, cervical, skin cancer and gastrointestinal cancer screening programmes and treatments; results in reduced referrals for common malignancies such as lung cancer; and increases prevalence of mental health conditions in the young and old. This is not to mention the many impacts on the economic determinants of public health. 14
General Impact on hospital system and elective care
It is difficult to estimate the burden of non-Covid morbidity and mortality during 2020 and to predict the effects in the years to come. An April report from the UK ONS indicated that it will far exceed the number of deaths observed with, or due to COVID-19 (in the region of 50,000 for the UK so far): “Various evidence supports the estimate that 75% of elective care has been postponed…If this activity were cancelled entirely it would result in an estimated 185,000 additional deaths.
This scenario does not account for other cuts to services that are known to have taken place already in many out-of-hospital services partially or fully, including NHS health checks, non-urgent primary care (dental and GP), de-prioritised community services, and some screening and vaccination programs”.15It is crucial to note that COVID-19 deaths sadly occur in people close to or above life expectancy age. In contrast, lockdown-induced deaths will occur in people well below the life expectancy age.
Therefore the “life years lost” as a result of lockdown could far exceed the number of those saved. Given that many publications demonstrate that lockdown has no significant impact on mortality – the life years lost due to lockdown will likely outweigh those saved by a huge factor. Striking data from Public Health England, detailed excess mortality trends for the months leading up to November 2020. 16No excess mortality was observed in the hospital or care home setting. In contrast, all of the excess mortality occurred in the “home” or “other places” (figure 6). In other words, the excess death for many months now, cannot be due to COVID-19, as the latter would dominate deaths in the hospital and care home settings. Rather, the inference is that excess death is now driven by the negative effects of lockdown itself.
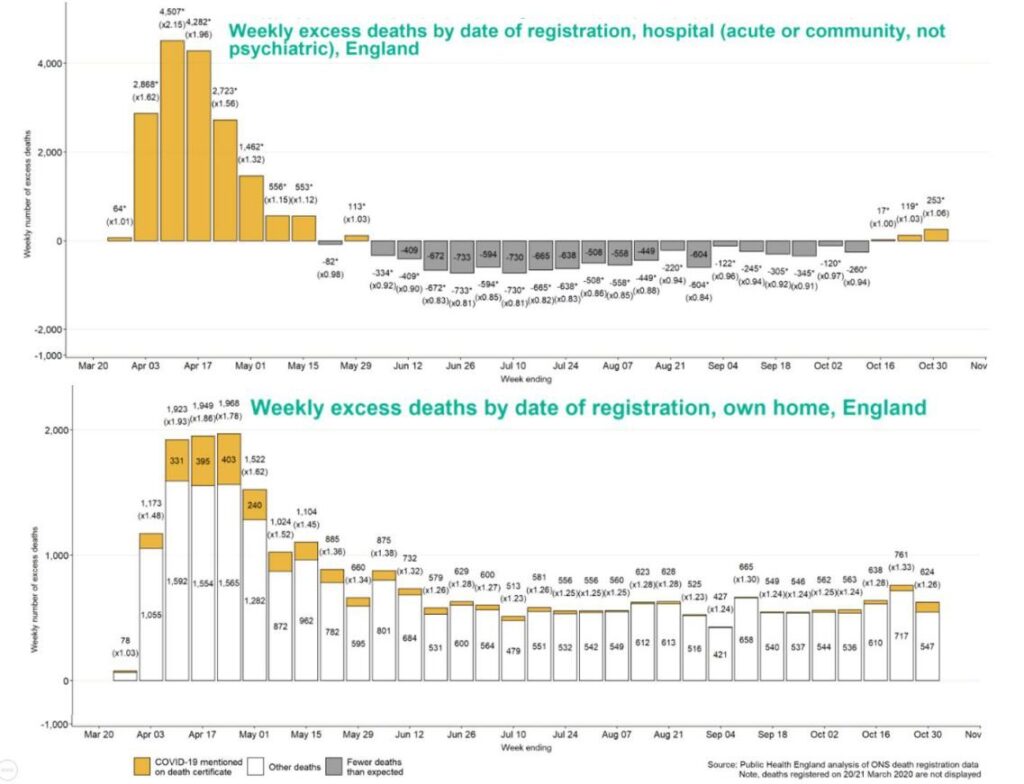
In further support of this, it is clear that the excess death is dominated by the 14-44 and 45-64 age groups, and largely absent from the more aged groups (figure 7). This is not the pattern of COVID-19 impact. We believe this pattern is consistent with lockdown-induced morbidity and mortality.

Lockdown Impacts on Cardiovascular Disease and Cardiovascular Events
Cardiovascular disease is the world’s biggest killer, and fatal events are strikingly affected by speed of access to proper care. Lockdown interventions have seriously impacted this care. There are many published analyses now summarizing the impacts.
For instance, a recent UK study “…recorded a 56% increase in the incidence of OHCA (out of hospital cardiac arrest) from 1 Feb to 14 May, versus 2019. Another study had similarly striking conclusions: “A retrospective analysis of 9 UK hospitals showed a decrease in admissions of 58% and a decrease in emergency department presentations of 53% after 23rdMarch 2020, when compared to the same period in 2019” 18.
Another study concluded: “Deaths in the home included 35% excess cardiovascular deaths” , while another stated the COVID-19 pandemic resulted “in an excess of acute cardiovascular deaths, nearly half of which occurred in the community”. These impacts of lockdown, for cardiovascular deaths alone – could potentially exceed the COVID-19 mortality impacts over the longer term.
Lockdown Impacts on Cancer Services
Cancer screening and treatment are additional crucial health pillars negatively impacted by the lockdown strategy. A recent UK paper captured the stark reality: “Results of COVID-19 disruption on cancer mortality range from 1,412 deaths for one month of assumed disruption to 9,280 deaths for six months of disruption20
Cancer screening has also been badly impacted: “the number of” performed CT scans dropped by 28% in April, May and June 2020 compared to the same time last year, with the additional challenge that CT scanning has been used to diagnose COVID-19.
MRI scanning has also decreased by 53%.”21Just one cancer type e.g. colorectal, could have very significant numbers of life years lost: “Delays of 2/4/6 months across all 11,266 patients with colorectal cancer diagnosed per typical year via the 2 week wait pathway were estimated to result in 653/1,419/2,250 attributable deaths and loss of 9,214/20,315/32,799 life years respectively”.22
Another report calls out the major impacts and future loss of life years in the balance: “the weekly number of cancers detected decreased by 58%. The proportion of missing cancers ranged from 19% (pancreaticobiliary) to 72% (colorectal)”.23The Irish Cancer Society published a submission to the Oireachtas on 17July, which laid out the grim impacts that lockdown would have on increased cancer death rates into the future.24As with cardiovascular disease, the impacts of lockdown, for cancer deaths alone – may exceed the COVID-19 mortality impacts over the longer term.
Lockdown Impacts on Mental Health
The effects of lockdown on those with mental health vulnerabilities must be one of the most concerning considerations in this debate. People affected by these issues are typically poorly represented in our society and are particularly vulnerable.
A study with more than 3000 subjects showed that increased psychological morbidity was evident in the UK as a result of the COVID-19 pandemic and found this effect more common on younger people, women and in individuals who identified as being in recognised COVID-19 risk groups.25Troubling as these findings may be, they are all the more concerning when it is considered that access to mental health services during a lockdown are grossly curtailed.
An Italian study observing the impact of lockdown on mental health services for migrants and individuals in socio-economic difficulty confirmed major difficulties in accessing these vulnerable populations during a period of time in which their mental health needs were expected to increase. Moreover, the reduction seen in follow-up compliance increased the risk of treatment discontinuation and possible relapse.26
A major study published in The Lancet Psychiatry identified groups in the population that had a high prevalence of psychological distress before the pandemic. As the economic consequences of lockdown developed, the authors proposed that it was reasonable to expect not only sustained distress and clinically significant deterioration in mental health for some people, but the emergence of well described long-term effects of economic recession on mental health including increasing suicide rates and hospital admissions for mental illness. Women, young people, and those with preschool aged children experienced the greatest increase in mental distress. 27The vulnerability of children and adolescents
is of major concern in lockdown scenarios – a rapid review of 63 studies showed that children and adolescents are more likely to experience high rates of depression and anxiety during and after enforced isolation ends. The duration of loneliness appeared to be a predictor of future mental health problems.28
Yet another major UK study with more than 12,000 participants showed that the percentage of participants classified as experiencing mental health problems increased from 23.3% in 2017-2019 to 36.8% in April 2020. In a multivariate mixed effects logistic regression model all population subgroups examined showed statistically significant increases in mental health problems. 29
Lockdown also has the effect of making the poor and most vulnerable in society suffer inordinately while increasing the gap between the rich and the poor. The destructive effects of lockdown are myriad, unemployment being one of the most corrosive outcomes. For example, in one study a 1-point increase in unemployment increased drug-related deaths by 3.3%.30The United Nations University WIDER Working Paper estimated an outcome of a 400-600 million persons increase in global poverty given a scenario in which per capita consumption contracts by 20%.31For context, New Zealand has already experienced a decline in GDP per capita of 12.6% by the end of q2 2020.32 There are now many published papers cataloguing these and other negative effects on population health.
A perusal of the website https://collateralglobal.org/ presents links to no less than 25 publications on adverse physical health impacts, 23 publications on adverse mental health impacts, and 29 publications on adverse social health impacts.
We believe that the lockdown strategy represents a very blunt instrument for management of the problems presented by COVID-19, and that it does so to the exclusion of too many of the other crucial facets of population health and wellbeing.
In summary, the evidence suggests that the lockdown strategy, while initially warranted, if pursued any longer, risks the worst cost-benefit outcome for any public health intervention in living memory.
Is PCR testing an appropriate tool to inform policy?
We are concerned about the implementation of PCR as the standard test for SARS-CoV-2. PCR has standard false-positive rates of 1- 3%33and up to 4% in the UK. 34 Suggesting that every positive PCR result constitutes an infectious “case”, is not accurate. For example, when the prevalence of COVID-19 infections in a population is relatively low – say 2% or so – the testing output would indicate that approximately 5% were “infected”. As the prevalence of infection declines, this ratio of false positives to true positives increases. This clearly misrepresents the real-world situation and has undue influence on important policy interventions. In addition, PCR cannot distinguish infectious live virus from residual dead virus or viral fragments from previous infection. Therefore many “cases” have no real meaning in terms of medical status or transmission potential – further misleading clinicians and policymakers alike.
The PCR test functions by amplification of tiny fragments of virus – “magnifying” them in a series of cycles. The number of cycles required to identify viral genetic material – the cycle threshold (Ct), correlates inversely with the amount of viral genetic material actually present in the original specimen.35363738
If there is little virus present, (probably not enough to be infectious) and the test has a high cycle threshold (cycle thresholds are set by the individual test kit manufacturers), it will probably identify harmless viral fragments and the test will be deemed “positive”. In Ireland, Ct value cut-offs of 35-45 are the norm.3339High Ct values (over 35 or even 30) suggest a non-infectious patient, often due to low viral load35 36 37 38 40(or the test identifying dead viral genetic 33, 34 4142,or often from contamination in the test process material from a previous infection ). In contrast, low Ct values are more likely to indicate a high viral load, and therefore an infection patient. 4336 37 44
We strongly suggest that PCR results are not considered in a binary positive/negative context.45 Clinical interpretation of the result, with the context of Ct values, would determine the potential to transmit infection46, or indicate the need for a repeat test4740. By this means, clinicians would have more insight when predicting outcomes for infected patients44and health authorities could be more focused, efficient and accurate when deploying contact tracing resources45.
Problems and inconsistencies with PCR testing have been documented extensively4833 41 42 4950: non standardised specimen collection techniques; no gold standard test yet identified; different tests used in different labs; no standardised acceptable Ct values; inconsistent quality assurance programs; false positives; identification of irrelevant dead viral genetic material which can persist for months after infection; potential contamination of specimens, to name a few.
Poorly designed PCR testing regimes can drive cases in infectious disease outbreaks and several reports exist of “pseudo” epidemics caused by over sensitive or poorly regulated PCR testing regimes. Patients with Ct values of >35 is extremely unlikely to be infectious unless they have been tested in the early stages of infection.
Repeat testing of such cases (with PCR or antigen techniques) should be standard, is consistent with existing HPSC policy, and would give clarity on their true status while use of techniques causing enzymatic degradation of dead viral genetic material, before PCR testing, could be explored as a way to distinguish previous from current infections.51
Proposing an evidence-based path forward
Removal of hard lockdown policy as a mitigation measure
- Focus on established, time-honoured pre-2020 epidemic management evidence-based principles (WHO, 2019 etc.)
- A functioning society is a healthy society – we consider lockdown to be dysfunctional and cyclical in nature with potential to render repeated harm on our society in the absence of a credible alternative approach. Reliance on lockdown strategy until such time as a vaccine is fully implemented and effective, would be unsustainable and an error in our view.
- Implement an updated epidemic/pandemic action plan that is Ireland-focused and can be used to address any such emergency in the future. The existing Ireland Pandemic Management Plan of 2019 could act as a ready-made template for such a reworked plan.
- Serious consideration of safe, workable, and reasonable proposals for the reopening of our education; hospitality; travel; tourism; sports and recreation sectors.
- Commensurate consideration of the mental and physical health impacts of COVID-19 mitigation measures so far, and strategies for their management.
2. Begin “intensive and focused protection of the vulnerable”
- Bring clarity on the use of PCR testing: policy around high Ct values and “weak positives”, repeat testing with or without rapid antigen tests, alignment of policy on PCR testing kits used nationally; clinical interpretation of all cases using Ct values; use of Ct values in identifying priority cases in the contact tracing system.
- Focus our testing resources – ideally rapid antigen (saliva sample) for workers engaged with high-risk groups – especially high-risk settings such as nursing homes, hospices etc. Introduce antigen testing pre-departure for passengers at airports and on arrival where deemed appropriate.
- The widespread deployment of suitable (e.g. N-95) face coverings to vulnerable groups and key workers.
- Government sponsored recruitment initiatives for at-risk workplaces such as nursing homes, with subsidies for wages and improved terms of employment (sick pay; rent allowances etc.)
- Regular testing (preferably antigen based) for workers in at-risk workplaces and carers of the vulnerable in the home.
3. Restoration of a functional health service
- Restoration of cancer screening and diagnostic services to pre-2020 levels
- Restoration of other key elective medical services such as cardiac screening services, orthopaedic joint replacement surgery and cataract surgery
- Policy for management of preventable lifestyle conditions that predispose to significant COVID-19 impact e.g. obesity, insulin resistance, vitamin D deficiency.
- Clarity around the timing and logistics for the safe implementation of a vaccine when it becomes available. Uncertainty around this issue will be detrimental to our progress out of this crisis.
- Realistic and implementable policies for staff recruitment (nurses and doctors) and increasing capacity of hospital beds and ICU beds in our hospital system.
4. Restore public morale and self-belief in the Irish population, empowering them to deliver solutions
- Re-establish the Oireachtas Special Committee on the COVID-19 response, to ensure legislative oversight for some of the most critical decisions faced by our country in many generations.
- NPHET daily briefings of ‘case’ numbers are open to misinterpretation and sensationalism by media – this in turn drives fear and concern among our population. We recommend that these briefings be stopped or reduced in frequency and that data be presented with context and perspective.
- We are deeply concerned by the absence of balance and debate in our media (print; tv; radio; social) around COVID-19 related issues and urge our leadership to consider and address this in a meaningful way.
- We must work together to update messaging and communication about COVID-19 to the people of Ireland: fear must be replaced with realistic information about actual risk in specific population groups; achievable goals, especially for our youth, which will have tangible benefits in the fight against the virus: hygiene; distancing; personal responsibility and empowerment.
- We encourage our Government to re-balance the emphasis in our health sector away from COVID-19 as its sole focus and towards the entirety of public health.
Ireland and her people have been well served by strong and consistent leadership throughout this unique and quickly evolving crisis. It would be a shame, after all our sacrifice and effort, to recall this challenging time not for our collective resilience, resolve and ingenuity but instead, for the lack of an agile strategy and a failure to recognize the challenges of COVID-19 in the context of broader socioeconomic and health policy. With openness to the best evidence and with balance in the ensuing debate, we can adapt our strategy to create the safest and most effective path forward for the people of Ireland. We look forward to assisting our political and scientific leaders in the pursuit of these common goals.
Original White Paper link with full academic references
Doctors & Medical Professional all Signatories
IF your Doctor’s name isn’t here, consider calling them and forwarding this page to them, and ask them to add their signature.
Initial Medical Signatories:
Prof. Jack Lambert, Mr. Martin Feeley, Dr. Alan Farrell, Mr. John Curran ,Dr. Vincent O’Carroll, Dr. James McDaid, Dr. William Ralph Dr. David Walsh Dr. Stephen Frohlich Mr. Maurice Collins Dr. Donal Collins
Dr. Andrew Rynne Dr. Ann McCloskey Dr. Wilma Lourens Dr. Michael McConville Dr. Gearoid O’Laoi Dr. Ailin Becker Dr. Sara Hunt Dr. Edgar Mocanu Dr. Arthur Cummings Dr. Peter A. Sloane Mr. Mihai VioreanuDr. Rupert Pollock Dr. Nigel Price
Twitter and Facebook have shut Freepress.ie down, please share this where you can – let’s spread the truth and take back reality.
Recent:
- Who Killed Garda Ray Ryan?…(substack)
- Mary Butler TD, Bill Kenneally, & the Deliberate Demolition of Child Mental Health Services – the Important Story O’Loughlin Tried to Bury…(substack)
- Covid Vax Terrorism – NATO’s New ‘Strategy of Tension’…(substack)
- Irish Refugees and State-Run Psychological Warfare – Katie Hannon & RTE…(substack)
- It takes ‘several months’ for a bank transfer from the 13.8 billion Apple-cash escrow account apparently…(substack)
- The Princess of Wales Kate Middleton’s cancer saga is an eminence front…(substack)
